
[ by Terri Lively ] – Original Article by Dental Products Report Here!
Dental sleep medicine is a field many practices are
taking on for its patient care and practice-building
opportunities. We spoke to experts in the area to get insight
into how to build a successful sleep practice.Millions of people have problems sleeping, and many spend a few minutes in your operatory at least once a year. Patients receive diagnoses of caries or gum disease, but what do they understand about bruxing, snoring, or sleep quality?
The American Sleep Apnea Association (ASAA) estimates 22 million Americans have sleep apnea, and 80% of them range from having moderate to severe cases of undiagnosed obstructive sleep apnea (OSA).1 Not only is sleep an area of medicine critical to patients’ well-being, but it’s also one that offers dental practices the opportunity to expand services and build practices. Dentists are well-positioned to diagnose and treat disordered sleeping.
Why Treat Sleep?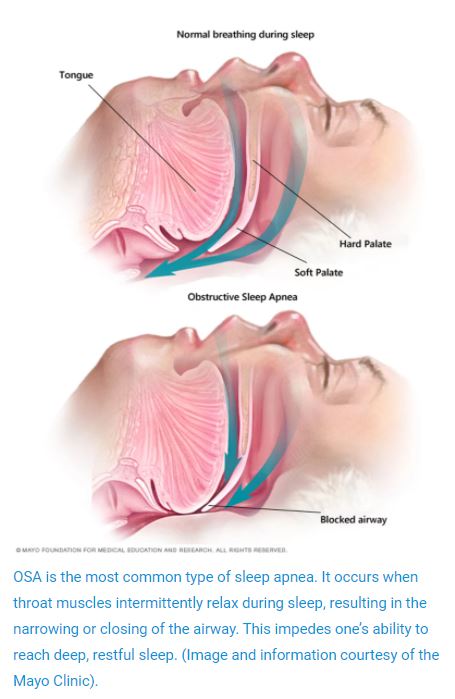 OSA happens when the airway is blocked, typically by the tongue collapsing against the soft palate, which causes the soft palate to collapse against the back of the throat, according to the ASAA. Left untreated, OSA can lead to severe health conditions, including high blood pressure, chronic heart failure, atrial fibrillation, stroke, and other cardiovascular diseases. Moreover, sleep apnea is associated with type 2 diabetes and depression and plays a role in causing traffic and heavy machinery accidents. Although OSA often presents in obese men aged over 40, the ASAA reports that OSA affects individuals of all ages, including infants and children.1
OSA happens when the airway is blocked, typically by the tongue collapsing against the soft palate, which causes the soft palate to collapse against the back of the throat, according to the ASAA. Left untreated, OSA can lead to severe health conditions, including high blood pressure, chronic heart failure, atrial fibrillation, stroke, and other cardiovascular diseases. Moreover, sleep apnea is associated with type 2 diabetes and depression and plays a role in causing traffic and heavy machinery accidents. Although OSA often presents in obese men aged over 40, the ASAA reports that OSA affects individuals of all ages, including infants and children.1
In 2017, the American Dental Association’s (ADA) House of Delegates adopted a statement about dentists’ role in treating sleep-related breathing disorders (SRBD).2 The ADA suggested that dentists play a vital role in a multidisciplinary approach to the care of patients with SRBDs. Moreover, the ADA says dentists are in an excellent position to identify at-risk patients. From medical and orthodontic referrals for children at risk for SRBDs to oral appliance therapy (OAT) for adult patients who have received diagnoses from a physician, the ADA recognizes dentists’ essential role in this effort.2
Dentists should consider adding dental sleep medicine to their practices because of a shortage of health care providers throughout the country, especially physicians outside large metropolitan cities, according to David Schwartz, DDS, president of the American Academy of Dental Sleep Medicine (AADSM) and a diplomate of the American Board of Dental Sleep Medicine (ABDSM)
Dentists have become more integral in patients’ overall health in recent years to compensate for this shortage. What dentists see and do in the operatory has a direct impact on the overall health of patients. Dr Schwartz says OSA is a prime example.
“We have a straight view of the airway with every patient we treat. It stands to reason that if we suspect OSA, we can quickly act to formally screen the patient, order a home sleep apnea test for appropriate candidates and then work with the patient’s medical provider to treat the disorder,” Dr Schwartz says.
Sleep apnea…is even more crucial to…the patient’s overall health than decay. Yet, as dentists, we are never trained about the significant impact we can make for that patient.”—Jonathan Greenburg, DDS
Neal Seltzer, DMD, FAGD, and Jeffrey Rein, DDS, FAGD, partners at Long Island Dental Sleep Medicine, recognize that OSA has been in the spotlight more recently because evidence links it to severe health complications. As “guardians of the airway,” dentists can save lives, Dr Seltzer says.
“We can help prevent someone maybe having a heart attack, high blood pressure, or getting in a car accident,” Dr Seltzer says. “That is the greatest impact we can have.”
Dr Schwartz, who has lectured on many aspects of dental sleep medicine, and authored and co-authored various articles, believes qualified dentists can have a positive impact on what he describes as a public health crisis. Moreover, treating OSA and snoring does not require new or specialized equipment investments, he says.
“It does require some investment in education and training, but the investment is not prohibitive,” he says.
Sleep is within the clinical scope of dental practices, according to Alice Limkakeng, CEO of SleepArchiTx, who says individuals with sleep disorders need immediate attention. In addition, because of the coronavirus disease 2019 (COVID-19) pandemic, treating patients for sleep disorders is vital to their health. Sleep comes in cycles, she says, and each sleep cycle accomplishes different tasks for our bodies, such as memory consolidation or releasing growth hormone. The deepest part of the sleep cycle, called N3 sleep, is where the body heals itself and rebuilds its immune system.3 This stage is essential for all patients, regardless of the virus, she says.
“If you’re snoring and having sleep apnea episodes, your sleep cycle is getting interrupted, and you never get to the deep stage of sleep where you rebuild and restore. Treating patients for sleep will increase the patients’ ability to rebuild their immune system and potentially protect them from COVID-19,” Limkakeng says.
Dentists are struggling right now and have patients who need their help with SRBDs, says Jonathan Greenburg, DDS, inventor of Zyppah, and founder and CEO of Sleep Certified. Just as a dentist would not ignore decay in a patient’s mouth, clinicians should not overlook OSA or evidence of other sleep-related disorders they observe in the oral cavity.
“Sleep apnea and severe snoring are even more crucial to the quality of care and a patient’s overall health and quality of life than that decay. Yet, as dentists, we were never trained about the importance and the significant impact we can make for that patient, and we should be addressing it,” Dr Greenburg says.
The Division of Sleep Medicine at Harvard Medical School lists many consequences of insufficient sleep. In the short term, patients can suffer changes in mood, decision-making, ability to learn and remember information, and increased risk of accidents or injury.4 In the long term, it can lead to obesity, diabetes, cardiovascular disease, and even early death.4 For all of these reasons, proponents of dental sleep medicine emphasize the benefits to patients the most.
“It’s about saving lives. It’s about adhering to the standard of care, doing the 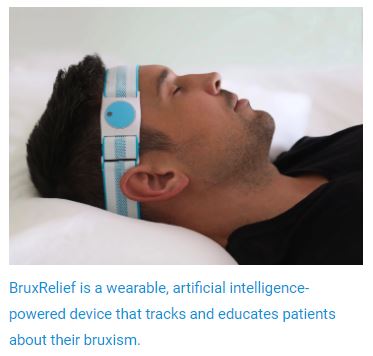 right thing, and giving back to your community,” Limkakeng says.
right thing, and giving back to your community,” Limkakeng says.
The connection between sleep and whole-body health is urgent, says Payam Ataii, DMD, MBA, co-inventor of the Aligner Sleep Appliance and clinical adviser to SleepArchiTx—so much so that he has put dental sleep topics at the forefront of his communication with patients and used these important health messages to reengage patients after the pandemic shutdown.
“The dentist should add sleep treatments to their repertoire because taking care of patients is what we do. This aspect of their health care is too important not to make ourselves better able to identify and treat these patients who have previously fallen through the cracks of our health care system,” Dr Schwartz says.
“If you care about your patients, sleep should be part of your practice,” Dr Greenburg adds.
topics at the forefront of his communication with patients and used these important health messages to reengage patients after the pandemic shutdown.
“The dentist should add sleep treatments to their repertoire because taking care of patients is what we do. This aspect of their health care is too important not to make ourselves better able to identify and treat these patients who have previously fallen through the cracks of our health care system,” Dr Schwartz says.
“If you care about your patients, sleep should be part of your practice,” Dr Greenburg adds.
Undiagnosed Bruxism
The ASAA describes sleep bruxism as a sleep-related movement disorder that results in a patient’s unconscious physical grinding of teeth while asleep.5 The symptoms of bruxism are often shared by patients who also have undiagnosed OSA, although, to date, the literature only suggests a correlation between the 2 conditions, not a causal relationship.5
Surveys suggest that 33% to 35% of patients have undiagnosed bruxism. I think that number is probably going up in this stressful pandemic era. There are signs of bruxism…right there in the oral cavity.”—Norman Hicks
Like OSA, there is a lot of undiagnosed bruxism. In a 2016 study published in the journal Sleep, the prevalence of regularly reported sleep bruxism was 8.6% for the general population.6 The Academy of General Dentistry (AGD) fact sheet on bruxism estimates that 1 in 3 people suffers from sleep bruxism, which they attribute to people with aggressive and competitive personality traits, and people who feel stressed, hurried, or nervous.7
“Surveys suggest that 33% to 35% of patients have undiagnosed bruxism,” says Norman Hicks, a consultant for GrindRelief Pro, a mouthguard for patients who clench and grind their teeth. “And I think that number is probably going up in this stressful pandemic era.”
Diagnosing and treating bruxism can build a dental practice and provide a new level of patient treatment that can reinvigorate dentists’ passion for dentistry. Plus, diagnosing bruxism does not require adding much to the daily routine.
“There are signs of bruxism that a clinician can see right there in the patients’ oral cavity, every day,” Hicks says.
According to the AGD, a dentist can easily diagnose bruxism, which includes the following signs:7
- Flattened appearance to the tips of the teeth
- Increases in sensitivity from the exposed dentin, resulting from grinding
- Jaw pain or popping in the temporomandibular joint
- Tongue indentations
When the Bravrr team started working on its BruxRelief product—a wearable artificial intelligence and health tracking device meant to educate patients about their bruxism—they learned that a significant problem in treating bruxism is patient acceptance, according to Bravrr CEO Brock Predovich. Patients do not always accept a bruxism diagnosis, and many think there must be another cause for the symptoms, he says.
“Really, the patient is objecting because they don’t want to spend $400 to $800 on a dental splint or night guard,” Predovich says.
Bravrr designed BruxRelief to help patients understand bruxism and the impact it has on their body, including symptoms such as neck pain, ringing in their ears, vertigo, and migraines. A patient wears the BruxRelief headband while sleeping. It captures and sends bruxism assessment data to the associated smartphone app. The data are shared with the patient and clinician to help them understand the clenching and grinding activities that occur when the patient is sleeping, including specifics about force, frequency of occurrence, and duration of bruxism events.
“It breaks it down into the nitty-gritty details,” Predovich says about the reports’ data. “BruxRelief is a tool that helps more patients get the help they need. Having a tool that will reveal more patients in a dental office that need help is another thing that we are excited to provide.”
BruxRelief addresses the trend for holistic treatment that patients want from their oral care team, Predovich added. Often, patients have complained about symptoms such as vertigo or migraines to their primary care physicians but do not mention them to their dentist. However, he says, the dental team could possibly relieve those symptoms faster than the medical team could.
Describing BruxRelief as a “Fitbit for bruxism,” Predovich says the team at Bravrr hopes it will increase patient awareness about how to get relief from their symptoms, adherence with bruxism treatment plans, and increased efficiency for the dental team when addressing bruxism with patients in the operatory.
Patient adherence in the area of bruxism is a challenge, Hicks agrees. Many bruxism relief devices that protect the patient while they sleep require impressions, models, lab work, and then fitting appointments, which can be time-consuming and expensive for patients. The GrindRelief Pro product, invented by Joseph Pelerin, DDS, of Advantage Dental Products, Inc, is an FDA-cleared, bisphenol A–free translucent thermoplastic device based on the nociceptive trigeminal inhibition device. The dental team can fit the patient in the office during the appointment and send the GrindRelief Pro product home with them. The product can reduce harmful muscle activity up to 60% because of its central power bar that prohibits the effect of teeth grinding on both arches, Dr Pelerin says.
time-consuming and expensive for patients. The GrindRelief Pro product, invented by Joseph Pelerin, DDS, of Advantage Dental Products, Inc, is an FDA-cleared, bisphenol A–free translucent thermoplastic device based on the nociceptive trigeminal inhibition device. The dental team can fit the patient in the office during the appointment and send the GrindRelief Pro product home with them. The product can reduce harmful muscle activity up to 60% because of its central power bar that prohibits the effect of teeth grinding on both arches, Dr Pelerin says.
How to Prepare for Sleep Treatment
It’s clear that treating SRBDs is part of a trend toward addressing patients’ overall health in dentistry that has been embraced by dental professionals and patients. Dental sleep medicine is a way to branch into more comprehensive care. But what should dentists do to prepare their practice for that leap?
This aspect of their health care is too important not to make ourselves better able to identify and treat these patients who have fallen through the cracks of our health care system.”
—David Schwartz, DDS
Long Island Dental Sleep Medicine, Seltzer and Rein’s practice, is currently 50% sleep medicine and 50% general dentistry. Deciding to branch into dental sleep medicine has a massive learning curve that requires research, education, and patience, both say. Dental schools spend an average of only 3.92 hours on sleep medicine education, so dentists should seek continuing education in sleep-related breathing disorders.8 However, Drs Seltzer and Rein also believe it is one of the most rewarding career moves for a dentist.
Both believe understanding the mouth, upper airway, and breathing is dentistry’s true calling. Dentists’ expertise about the oral cavity makes them “the most qualified of all health care providers to provide this remarkable service,” Dr Seltzer wrote in the American Sleep and Breathing Academy’s Sleep and Wellness magazine.9
 Drs Seltzer and Rein credit digital technology for making OAT more successful in treating SRBDs. Their practice uses Dentsply Sirona’s digital suite of technology, such as the CEREC scanner and the Axeos CBCT, to plan treatment and collaborate with the sleep lab on the design of oral appliances.
Drs Seltzer and Rein credit digital technology for making OAT more successful in treating SRBDs. Their practice uses Dentsply Sirona’s digital suite of technology, such as the CEREC scanner and the Axeos CBCT, to plan treatment and collaborate with the sleep lab on the design of oral appliances.
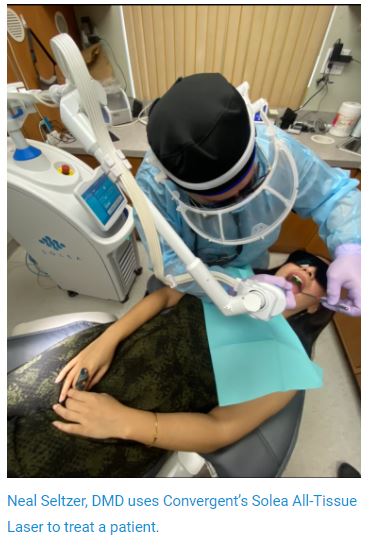
In addition, they have invested in Convergent Dental’s Solea All-Tissue Laser. The Solea has a proprietary wavelength that targets the collagen layer in the soft palate, enabling it to “tighten up,” according to Dr Rein, who says the Solea is easy to use. Plus, it creates minimal sensation for the patient, so it’s an easily tolerable procedure, and the Solea requires fewer visits for treatment than the competition, which makes it more economical for the patient, he adds.
Their practice also uses the Solea laser to provide painless, anesthesia-free removal of decay, according to Dr Seltzer.
Although dentists can treat SRBD, only a licensed medical provider can diagnose sleep apnea or snoring. However, dentists can screen for sleep apnea and snoring, order or administer a home sleep apnea test in most states, and provide OAT once a licensed medical provider has diagnosed sleep apnea or snoring and prescribed treatment, Dr Schwartz explains.
However, treating patients with OSA or snoring requires continuing postdoctoral education, training, clinical judgment, collaboration with medical colleagues, excellent patient care, and an understanding that the team is treating a medical disorder, he adds.
“Improper treatment of OSA exposes patients to potentially life-threatening outcomes,” Dr Schwartz says. “Dentists who treat OSA without proper education are exposed to serious medicolegal responsibility should either accident or disease lead to one of these outcomes.”
Recognizing this need, the AADSM, the leading national organization representing dentists who treat sleep-disordered breathing with OAT, developed the AADSM Mastery Program. Although offered through AADSM, the mastery program is also available through accredited dental school continuing education (CE) programs, such as Tufts University. The AADSM Mastery Program is a comprehensive, clinically focused, and evidence-based education program that provides dentists with the training and skills they need to provide OAT to patients who suffer from OSA and snoring. Upon completion, dentists have the competence and confidence to provide OAT and build relationships with patients, physicians, and payers, Dr Schwartz says.
“The AADSM Mastery Program is also a pathway for dentists to become AADSM Qualified Dentists, as well as diplomates of the American Board of Dental Sleep Medicine,” he adds.
Every dentist should screen for OSA in their patients’ initial exams and then refer to a medical professional who can deliver proper diagnoses, Dr Seltzer says. Both he and Dr Rein have spent the last 3 decades developing relationships with physicians who refer to them. Both dentists agree that the education that accompanies taking on dental sleep medicine is essential to forging these relationships.
“We treat OAT similar to becoming a specialist in other fields of dentistry,” Dr Seltzer says regarding learning about SRBD and OAT, pointing out that this additional education goes a long way with the medical community. “Most physicians want to put their patients in the hands of a qualified medical person.”
Drs Seltzer and Rein say patient adherence is one of the challenges of successful treatment outcomes for sleep apnea. Continuous positive airway pressure (CPAP) machines are often considered the gold standard for treating sleep apnea, but many patients find them difficult to use and eventually give up.
“OAT is most effective in treating mild to moderate sleep apnea but has shown to be successful with some severe cases as well,” Dr Seltzer says.
“While the CPAP is the frontline defense for severe OSA, the ease of [adherence] can make oral appliance therapy more effective over time,” Dr Rein says.
OAT is vital during COVID-19. Dr Schwartz says providing OAT does not generate aerosols and allows for some appointments to be conducted with telehealth. Limkakeng agrees, adding that early this year, the AADSM and American Academy of Sleep Medicine stated that medical professionals should prescribe OAT rather than the traditional CPAP machine, which forces air and increases the risk of transmission.
Limkakeng agrees that preparing to treat patients with dental sleep therapy is a lot more than taking CE courses on the clinical aspects and learning about different devices. Although that is part of it, the clinical component is the easiest part for dentists, she says. Appropriate treatment also needs systems and processes in the offices to address different areas, which go along with providing the highest quality of care. For example, she recommends having a consistent program to ensure that you screen all patients.
“There are a lot of practices out there dabbling in dental sleep medicine and cherry-picking patients that they believe might have a sleep disorder, and that’s a first step,” Limkakeng says. “But in terms of adhering to the standard of care and getting objective data to help you determine who needs therapy, screening every patient is the way to do it because the old thought that only middle-aged obese men suffered from sleep apnea has been long demystified. Your day-to-day dental patient that appears healthy often surprises practices when they are diagnosed with sleep apnea.”
Limkakeng also recommends collaborating with medical providers to get the appropriate, high-quality diagnosis done. Moreover, she wants practices to prepare patient education and communication on what this disease is, why it is essential to get treated, and how it relates to overall health. Finally, to support the financial side, she suggests collecting information on documenting the treatment appropriately for medical insurance reimbursement.
to prepare patient education and communication on what this disease is, why it is essential to get treated, and how it relates to overall health. Finally, to support the financial side, she suggests collecting information on documenting the treatment appropriately for medical insurance reimbursement.
“Individually, these are not hard tasks, but collectively there are several different things that I believe need to be prepared in addition to the clinical aspects to have a high-quality program and treat your patients appropriately,” Limkakeng says. “That’s why we have designed SleepArchiTx to be a 1-stop-shop partner to handle all of these aspects of medical doctor diagnosis coordination, patient communication, and medical billing for dental practices.”
According to Dr Greenburg, there are 2 tracks dental professionals could take to add sleep to their practice. One track is to start with CE and other training courses and to include the entire staff. Dr Greenburg says that dental professionals should get information from several different types of programs to get a good foundation in dental sleep science.
“However, that’s a traditional track that takes a lot of time,” Dr Greenburg says.
The second track he recommends is to outsource the logistics to a third party. There are a few companies, including Dr Greenburg’s new Sleep Certified 360 program and Limkakeng’s SleepArchiTx, that help practices get over the barriers for sleep therapy. These third-party companies handle details like arranging for sleep testing, coordination with physicians, and billing medical insurance for therapy, among other obstacles and administrative tasks.
“You’re going to have those that want to specialize and take a greater interest, and they will go the traditional route,” Dr Greenburg says. “But we anticipate the bulk of practices are going to go in this new direction because it’s so challenging for people to get past these hurdles.”
What Makes a Practice Successful?
Getting educated and excited about treating anything new in the dental office is only the first step, according to Jon Caulfield, DDS, who runs a practice in Littleton, Colorado. Implementing change and getting buy-in from the team are the next, and Dr Caulfield says it can be like “pulling teeth.” The most successful offices create a culture of excitement and passion for treating sleep, with an appreciation of the important role it plays in health. Dr Caulfield says having every member of your team engaged and accountable in the mission makes a big difference when you begin something new. Plus, he says, working with experienced partners, such as Vivos Therapeutics, can make the transition much easier.
“When I began working with Vivos Therapeutics, the entire team was involved and engaged and could see the bigger picture and how we were making a difference in the sleep and lives of our patients,” Dr Caulfield says. “They helped us define the systems and the processes and the roles that we would all get to play and made it possible by providing the resources and guidance to fulfill those roles. Having advisers for the practice, the marketing, and the clinician made the transition and integration much easier for my team and myself. I could take the time I needed to learn the treatment aspects of sleep while my team was educated and empowered to run the business and logistics of treating sleep in the dental office.”
Limkakeng found that the most successful dental sleep medicine practices are systematic with the effort and incorporate it into the workflow. Providing therapy with 1-off cases is difficult and time-consuming, she says, but once you have a process, and are screening every patient, a successful sleep practice will follow. She also says dedicating a staff member to this effort or working with an outsource partner who will help them implement and support their dental sleep medicine practice daily is essential because most successful sleep practices make sleep therapy part of their everyday routine. Additionally, patient education is key, she says.
Patient buy-in is critical, Dr Ataii agrees. “We doctors know all the clinical complexities, but we are often not great at translating that to something patients can understand. Working with outside partners like SleepArchiTx or others to get patient education videos and brochures is essential to getting patients to accept treatment.”
Dr Seltzer recommends getting your credentials. Drs Seltzer and Rein are  both diplomates of the ABDSM, Academy of Clinical Sleep Disorder Disciplines, and the American Sleep and Breathing Academy. They each have 30 years’ experience in sleep medicine and are proud to be the first office in New York state to be a Dental Sleep Medicine Accredited Facility by the AADSM. Credentials build credibility with medical doctors and patients, Dr Seltzer says.
both diplomates of the ABDSM, Academy of Clinical Sleep Disorder Disciplines, and the American Sleep and Breathing Academy. They each have 30 years’ experience in sleep medicine and are proud to be the first office in New York state to be a Dental Sleep Medicine Accredited Facility by the AADSM. Credentials build credibility with medical doctors and patients, Dr Seltzer says.
“It gives the patient the understanding that not only the doctor is good, but also the whole facility is credentialed,” he says. “These standards make it so the patient knows that they’re going to a very highly regulated and professional office that’s going to meet all the criteria so that they are treated well.”
Hicks agrees that education is paramount to treating SRBDs. In February 2021, their GrindRelief Pro team plans to release new CE through the Catapult Education program that addresses bruxism diagnosis and treatment. Their first CE program will present the clinical signs to look for and the science behind this therapy.
“A lot of dentists need that science before they’re even comfortable saying anything,” Hicks says.
Within his general, restorative dental practice in the Chicago area, Dr Schwartz has focused on dental sleep medicine for more than 22 years. He is also the director of dental sleep medicine at The Center for Sleep Medicine, a multidisciplinary sleep center with several locations in the greater Chicago area. He agreed that education for dentists, staff, and patients is essential.
“Only through appropriate professional education and patient education can we build confidence, not only in what we do but also in how our treatment impacts our patients’ overall health,” Dr Schwartz says.
“You have to remember that this is all about case acceptance. You need patient buy-in. If there’s one thing that practices should get help on, it is case acceptance,” Limkakeng says. “Make sure you have a partner who can help you with patient education and communication, and acceptance materials.”
Dr Greenburg says the most successful sleep practices are not afraid to try new things and commit to them. He says most dentists understand that when you get into a new area of treatment, whether that is placing dental implants, implementing CEREC, or now treating sleep disorders and OAT, it is overwhelming at first. However, if you push through those overwhelmed feelings, you will gain confidence.
“Anything worth having, you have to work for,” Dr Greenburg says.
References
- Sleep apnea information for clinicians. American Sleep Apnea Association. Accessed November 29, 2020. https://www.sleepapnea.org/learn/sleep-apnea-information-clinicians/#:~:text=A%20very%20short%20course%20on%20sleep%20apnea&text=Sleep%20disorders%2C%20including%20sleep%20apnea,severe%20obstructive%20sleep%20apnea%20undiagnosed.%20Accessed%20November%2029,%202020
- The role of dentistry in the treatment of sleep related breathing disorders. American Dental Association. Accessed November 25, 2020. https://www.ada.org/~/media/ADA/Member%20Center/FIles/The-Role-of-Dentistry-in-Sleep-Related-Breathing-Disorders.pdf?la=en
- Nasca TR, Goldberg R. The importance of sleep and understanding sleep stages. American Sleep Apnea Association. Accessed November 25, 2020. https://www.sleephealth.org/sleep-health/importance-of-sleep-understanding-sleep-stages/#:~:text=N3%20sleep%20is%20a%20regenerative,measured%20N3%20sleep%20at%20night
- Consequences of insufficient sleep.
Division of Sleep Medicine at Harvard Medical School. Accessed November 26, 2020. http://healthysleep.med.harvard.edu/healthy/matters/consequences - If you grind your teeth at night, you might have sleep apnea. American Sleep Apnea Association. July 2, 2017. Accessed November 29, 2020. https://www.sleepapnea.org/if-you-grind-your-teeth-at-night-you-might-have-sleep-apnea/
- Khoury S, Carra MC, Huynh N, Montplaisir J, Lavigne GJ. Sleep bruxism–tooth grinding prevalence, characteristics and familial aggregation: a large cross-sectional survey and polysomnographic validation. Sleep. 2016;39(11):2049-2056. doi:10.5665/sleep.6242
- What exactly is bruxism? Academy of General Dentistry. Accessed November 29, 2020. https://cfdds.com/images/pdfs/bruxism.pdf
- Simmons MS, Pullinger A. Education in sleep disorders in US dental schools DDS programs. Sleep Breath. 2012;16(2):383-392. doi:10.1007/s11325-011-0507-z
- Seltzer N. Dentistry’s hidden calling “the airway.” American Sleep and Breathing Academy. August 20, 2020. Accessed November 25, 2020. https://asba.net/dentistrys-hidden-calling-the-airway/